Internal Carotid Artery Occlusion at its origin from the common carotid or intracranial is the site of the major vascular lesion in nearly 20 per cent of strokes. The usual lesion is atherosclerotic with, at first, partial obstruction and, finally, occlusion with a thrombus. Occasionally the internal carotid artery is obstructed by a large embolus.
Symptoms And Signs of Internal Carotid Artery Occlusion
Symptoms and signs specific for internal carotid artery occlusion in the neck are intermittent visual impairment or blindness in the eye on the side of the occlusion (retinal artery insufficiency combined with a contralateral hemiparesis and sensory loss (middle cerebral artery insufficiency). This clinical picture often begins with a series of transient ischemic attacks and only later causes permanent weakness and sensory loss. Unless the history of intermittent blindness can be obtained, it is difficult, on clinical grounds alone, to distinguish occlusion of the internal carotid artery from middle cerebral artery occlusion.
On neurologic examination, patients with cerebral infarction due to internal carotid artery occlusion have paresis of voluntary movement, with weakness most noticeable in the contralateral face and upper extremity. Infarcts usually produce motility defects as their main manifestations, but there is usually some impairment of sensory perception and, at times, visual field impairment as well.
In the paretic extremities, deep tendon reflexes are hyperactive, and pathologic reflexes such as the Babinski sign (extensor plantar response) are found. Muscle tone becomes increased on the weakened side, and spasticity may be so marked that early contracture is evident. Sensory impairment is most evident in modalities such as position sense, vibration sense, two-point discrimination, and tactile perception of shape and texture. Touch and pain perception may be moderately impaired, and extinction of stimuli on the involved side may be evident on double simultaneous stimulation.
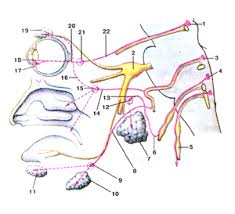
The size of the cerebral infarction produced by internal carotid occlusion is extremely variable. When there is no collateral circulation through the anterior communicating, posterior communicating, ophthalmic, or surface collateral arteries, the infarct can involve nearly the whole cerebral hemisphere, both lateral and medial surfaces. With a richer collateral circulation, smaller infarcts and proportionately fewer neurologic defects result. Occasionally occlusion of the internal carotid is asymptomatic, and is discovered only ‘as an incidental finding at autopsy or when cerebral angiograms are done.
Internal carotid artery occlusion or stenosis sometimes causes a partial Horner’s syndrome (slight ptosis and miosis) on the side opposite the paresis. The eye changes have been attributed to ischemia of the sympathetic fibers that lie in the adventitia of the arterial wall adjacent to the occlusion, but are more probably due to direct hypothalamic damage, for they can also be observed in patients with similar infarcts who do not have occlusion of the carotid arteries. An audible bruit in the neck at the angle of the mandible is a helpful indicator of stenosis of the internal carotid artery at that site.
Occlusion of the internal carotid artery is also’ suggested when the retinal artery pressure on the affected side, as measured with an ophthalmodynamometer, decreases 25 per cent or more below the arterial pressure in the other eye. Some physicians find that palpation of the internal carotid artery in the pharynx behind the posterior tonsillar pillar is helpful in the diagnosis of carotid artery disease, as the pulse is absent when the artery is occluded. However, patients are often unable to cooperate for the examination, so that the usefulness of the test is
limited.