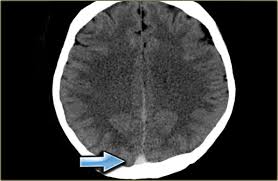
The symptoms of local cerebral venous thrombosis are headache, delirium, drowsiness, diplopia, and convulsions. The signs are usually those of increased intracranial pressure with papilledema and focal neurologic abnormalities. Focal fits are common, as are paresis and hemisensory’ loss. Such patients are restless, confused, and obtunded.
Superior sagittal sinus occlusion produces a somewhat similar clinical picture. At the New York Hospital, 21 patients with noninfective sagittal sinus thrombosis have been studied. Nine had terminal disease and marasmus, six had cyanotic congenital heart disease, and four had other, unexplained episodes of venous or arterial thromboses. Eleven of the 21 patients were children. Below the age of 10, cerebral infarction is more often due to venous than to arterial occlusion. Nearly all patients had fever, and their cerebrospinal fluids were under increased pressure, averaging 260 mm. of fluid, and contained more than 10 red blood cells.
Neurologic Symptoms appeared abruptly or progressed rapidly to a maximum, usually within 36 hours. Most patients were obtunded or confused and had headache. The white blood count was elevated in 10 patients; in 7 it was over 20,000. Nuchal rigidity was common, and papilledema, hemiparesis, and focal epileptic seizures occurred in about half the cases. Two patients presented later with signs of pseudotumor cerebri. The occurrence of hemiparesis or focal epilepsy was usually associated with cortical venous thromboses in addition to the sinus occlusion.
Cavernous sinus occlusion, usually a complication of sinus or paranasal skin infection, is characterized by proptosis, orbital chemosis, and edema, pain around the eye, papilledema, retinal hemorrhages, and fever. Extraocular palsy may be present. The disease carries a high risk of spread to the opposite cavernous sinus. Complications include meningitis and brain abscess.
Transverse or lateral sinus thrombosis, usually secondary to mastoiditis, is now uncommon with the decline in the incidence of that disease. When it does occur, it is usually manifested by headache, tenderness over the mastoid process, and, occasionally, paresis of the structures supplied by the glossopharyngeal and accessory nerve, with dysphagia, dysphonia, and weakness of .the ipsilateral sternomastoid and trapezius muscle.
In all varieties of cerebral venous thrombosis, there is usually some evidence of sepsis with fever, malaise, headache, and leukocytosis.
Although the condition is uncommon, a diagnosis of cerebral venous thrombosis should be kept in mind for patients with evidence of cerebral infarction who have focal seizures, increased intracranial pressure, or evidence of infection. Cerebral venous thrombosis is particularly likely as a cause of postpartum cerebral infarction.
The general evaluation of the patient with cerebral infarction usually reveals evidence of vascular disease at other sites as well as a variety of associated diseases. About one fifth of patients with atherosclerotic cerebral infarction in the Cornell-Bellevue series had previous strokes, half of which had occurred in the preceding year. Another fifth had had myocardial infarction, usually within the previous year. Over one half of the patients were hypertensive, but the diastolic pressure was above 100 mm. of mercury in only one third of the patients. Nearly one fifth of the patients had diabetes mellitus, and one in ten gave a history of peripheral vascular occlusive disease.
Physical Examination of Cerebral Venous Thrombosis
The physical examination of – most patients with cerebral infarction discloses a normal or slightly elevated body temperature. Careful examination of the heart should never be overlooked because the presence of cardiac enlargement, atrial fibrillation, and cardiac murmurs, suggesting rheumatic heart disease with mitral stenosis, aids in detecting the presence of cerebral emboli. Patients with cerebral infarction often have atherosclerotic coronary heart disease, and perhaps one fifth have had recent or associated myocardial infarcts.
Palpation may reveal absence of pulsation in easily felt peripheral arteries. In the lower extremities, this is indicative of atherosclerotic.
vascular disease in the aorta, iliac, femoral or popliteal arteries. In the upper extremities, it may indicate occlusions in the major branches of the aorta, such as the innominate or subclavian arteries. Absence of pulses in one or both upper extremities should alert the physician to such diagnoses as “pulseless disease” (Takayasu’s syndrome) or the “subclavian steal syndrome.”
Auscultation for bruit over the neck is helpful in identifying sites of extracranial stenosis. A bruit heard in the neck under the angle of the mandible suggests atherosclerotic disease of the carotid artery, and bruit heard just above the clavicles is associated with vertebral or subclavian artery stenosis. Bruit, when loud and localized, is associated with atherosclerotic obstruction at that site in more than three fourths of patients.
Laboratory Examinations. Laboratory tests are aimed, at both confirming the diagnosis and identifying complications. Every patient suspected of stroke should have a lumbar puncture and skull roentgenograms, and, if there are any unusual features at all about the illness, an electroencephalogram (EEG) should be obtained.
The cerebrospinal fluid should be examined promptly, for there is no other way to determine the presence of intracranial bleeding or an unsuspected infection. The lumbar puncture must be approached cautiously, however, when patients are in stupor or coma or when it is uncertain whether the illness is caused by stroke or by brain tumor, with increased intracranial pressure. In such instances, it is preferable to proceed with roentgenograms, electroencephalogram, radioactive brain scan, or an arteriogram, since lumbar- puncture can inadvertently precipitate tentorial or foraminal herniation when there is an expanding intracranial mass.
The cerebrospinal fluid pressure is rarely over 200 mm. of CSF in cerebral infarction. The fluid is usually clear and colorless, but bleeding and xanthochromia from hemorrhagic infarction may be found. The CSF protein level is usually normal although slight elevations to 60 to 75 mg. per 100 ml. are found in perhaps one fifth of the patients. Elevations to 80 mg. per 100 ml. or above are found in less than 10 per cent, but particularly in those with basilar artery disease. With massive cerebral infarction, the protein may be raised to values of nearly 100 mg. per 100 ml. Although diabetes occasionally accounts for pronounced CSF protein elevations with stroke, patients with high values should always be carefully reviewed for the possibility of brain tumor.
Skull roentgenograms should be examined for evidence of fracture, erosion of the posterior clinoids (suggesting chronically increased intracranial pressure), abnormal calcification, and pineal shift.
The electroencephalogram (EEG) offers potential help both in differential diagnosis and in distinguishing infarction of the brainstem from that of the hemispheres. The EEG is usually abnormal in patients with cerebral infarction, and the degree of abnormality generally parallels the size of the lesion and the severity of the neurologic deficit. With hemispheric lesions, the abnormality is focal and the normal frequency of brain waves is slowed, s
that, acutely at least, the records may resemble those found with brain tumor. In infarction, however, a decrease in the’EEG abnormality is expected in serial recordings as the patient improves. With brainstem infarction, the EEG may be entirely normal, paroxysmally abnormal, or generally and diffusely abnormal.
The general evaluation of patients with cerebral infarction should include an electrocardiogram (ECG) and a chest roentgenogram. The ECG may confirm the presence of an arrhythmia or may disclose a silent myocardial infarction. (A potentially confusing point is that the ECG may show minor T wave and S-T segment changes caused by cerebral infarction and not by primary cardiac dis ease.)