Demyelinating disorders must be considered as a basic disorder of the oligodendrocyte or the Schwann cell. To consider demyelination solely as myelin breakdown, ignoring the fact that the myelin lamellae are an integral part of the parent glial cell, may be contradictory to the pathogenesis. The etiologic agent may attack either the perikaryon of the glial cell or its plasma membrane to produce demyelination.
Prior to a consideration of the pathogenesis of demyelinating disorders, one must make some attempt to classify the varied primary disorders of myelin. In .1957 Poser suggested classification into two basic types. One, a so-called “myelinoclastic” or demyelinating type, includes disorders in which myelin forms normally to a certain age and then for unknown reasons breaks down. This includes the most common demyelinating disease, multiple sclerosis, and also acute disseminated encephalomyelitis and certain other disorders. The other, the “demyelinating” type, includes disorders in which a presumed inborn error of metabolism results in defective myelin formation. The category includes the so-called leukodystrophies or some of the diffuse scleroses and lipidoses of the nervous system and the aminoacidurias.
Pathogenesis.
In most demyelinating disorders, the cause remains unknown. Demyelin- zation is the typical response of white matter to noxious stimuli not severe enough to cause complete necrosis of the tissue, and almost any infectious, nutritional, vascular, or toxic disorder can result in demyelination. At present there is insufficient evidence to incriminate any one cause. However, the majority of workers interpret present evidence as supporting most strongly an allergic basis for most of the primary demyelinating disorders, with genetic and geographic factors influencing susceptibility. Autoradiographic studies in experimental allergic encephalomyelitis using tritiated precursors of DNA, RNA, and protein have shown a rise in circulating plasma-like cells prior to onset of neurologic signs. Supernatant from cultures of these cells produces demyelination in tissue culture of rat cerebellum similar to that produced by serum from multiple sclerosis patients.
Because of the wide divergence in their symptoms, the demyelinating disorders are grouped according to pathologic similarities that have been previously described. Within this framework further similarities have emerged between certain demyelinating disorders. The pathologic pictures :: rabies postvaccinal encephalomyelitis and parainfectious encephalomyelitis are almost indistinguishable. This resemblance has stimulated many experimental studies and has provided a starting point for investigation.
It has long been known that a certain fraction of physical treatments, indicating that it is probably patients who receive. antirabies treatment develop a neurologic syndrome called rabies postvaccinal encephalomyelitis (post immunization encephalomyelitis). In the immunization therapy of rabies, the patient usually receives 14 daily subcutaneous injections of killed rabies virus in a suspension of rabbit brain tissue. Encephalitis, or paralysis, if it occurs, develops any time from a week after the first inoculation to two weeks after the last.
There was much speculation that this complication was due to the virus until Rivers and co-workers in 1933 showed that multiple injections of normal rabbit brain tissue in monkeys resulted in encephalomyelitis with lesions similar to those seen in rabies postvaccinal encephalomyelitis. This was followed by the extensive investigations of Kabat, Wolf, and co-workers in the 1940’s, who demonstrated that experimental allergic encephalomyelitis (EAE) could be produced in monkeys by a few injections of adult homologous, heterologous, or autologous central nervous system tissue mixed with paraffin oil and killed mycobacteria (Freund’s adjuvant.’ White matter appeared more encephalitogenic than gray, whereas peripheral nerve and fetal unmyelinated) brain were ineffectual as encephalitogenic.
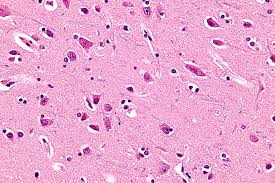
The encephalitogenic is stable to heat and other not a transmissible infectious agent, EAE is not transferable to other animals by serum, although the serum contains complement-fixing antibodies to brain. The pathologic change is primarily in the white matter of the central nervous system, with, perivascular arid meningeal inflammation and demyelination. These findings are in many instances indistinguishable from those in certain human demyelinating disorders. The cerebrospinal fluid’in acute EAE shows pleocytosis with elevation of gamma globulin content similar to the changes in many cases of demyelinating disorders in humans. Finally it has been demonstrated that cortisone administered prior to immunization prevents the development of EAE.
This classic pioneering work has been followed by genetic, immunologic, biochemical,»and ultra- structural investigations. It has been shown that there are variations in susceptibility to EAE among various species and strains within species. One inbred strain of mice was shown to be 100 per cent susceptible to induction of EAE, and another strain was shown to be 100 per cent resistant. A genetic analysis revealed that resistance was due to two pairs of resistance-conferring genetic factors. Other workers have successfully transferred EAE by means of sensitized lymphoid cells in isologous (inbred) strains. Finally, workers have found that serum from EAE animals or from some patients with multiple sclerosis causes destruction of myelin in cultures of transplanted brain tissue.
The nature of the encephalitogenic in EAE has been extensively studied., and most work indicates that it is a basic protein of myelin (Kies and Alvord, 1965). Specifically sensitized lymphocytes are found in immunofluorescence studies to take up this myelin protein. Other investigators showed that the delayed type of skin reactivity to the myelin protein correlates well with the onset and severity of EAE. Drugs other than cortisone (6-mercaptopurine or methotrexate), which depress lymphoid activity, and irradiation Of draining lymph nodes prevent the development of EAE. Serum from animals that have recovered from EAE has been shown to contain IgM antibody, which when transferred to recently sensitized animals prevents the development of EAE. The demyelination in EAE has recently been shown in electron microscopic studies to be a result of the phagocytosis of oligodendroglial cells and dissolution of the myelin lamellae by mononuclear cells.
The relationship of EAE to the spontaneous demyelinating disorders is still conjectural. Since the brain lacks a lymphatic drainage, myelin antigens are inaccessible to the body’s reticuloendothelial system. It is plausible to assume that in certain situations the body could produce myelin autoantibodies (cellular or humoral) that would react with central nervous system myelin and produce demyelinating lesions. How the normally inaccessible myelin autoantigens reach the antibody-forming site and under what circumstances this occurs are still unknown.