Venezuelan Equine Encephalitis is a Subsequent study of the virus by Casals and others established an antigenic relationship with Western and Eastern equine encephalitis viruses that places it, along with these, in arbovirus group A.
Although no etiologic association with human disease was recognized at that time, retrospective epidemiologic and serologic assessments indicate that these Guajira eruptions gave rise to extensive human infection with Venezuelan equine encephalomyelitis (VEE) virus in Venezuela in 1941 and 1942, manifested as an influenza-like illness that was abruptly terminated when effective measures for epidemic malaria vector control were introduced.
Human cases and fatalities were reported by Randall and Mills during the Trinidad equine epizootic of 1943-1944, which is now considered to have been an extension of the widespread epizootic-epidemic in Venezuela that immediately preceded that period. Although isolation of VEE virus from human brains in the Trinidad cases was reported, these strains have been lost. Numerous strains have been isolated from human laboratory infections resulting from handling viruses isolated from naturally infected equines.
The predominant manifestation of human infection with VEE virus as an influenza-like respiratory type of illness created doubt whether VEE virus, in fact, produced overt central nervous system disease in man. Subsequently, a number of epidemics resulting from natural exposure in Colombia, Panama, and Venezuela have yielded many VEE virus strains from brain and blood in humanS cases of acute febrile central nervous system disease.
Epidemiology.
When transmission to man occurs, VEE virus produces the highest incidence of overt disease —albeit influenza-like rather than encephalitic in nature —of any. mosquito-transmitted virus so far known. Central nervous system involvement probably does not occur in more than 3 per cent of the clinical cases, at most half of these terminating fatally. Nevertheless, the epidemic occurrence of tens of thousands of cases, as were reported from Venezuela during the period 1962- 1964, produced a significant enough number to represent the most serious recognized arbovirus encephalitis in Latin America.Venezuelan equine encephalitis is now considered to. be a pan-Caribbean arbovirus disease, evidence of human infection and isolation of virus strains being reported from Florida and Mexico in addition to the previously recognized human morbidity in Panama, Colombia, Venezuela, Trinidad, Brazil, Ecuador, and Peru.
Such a wide geographic distribution involves a variety of ecologic situations that range from sea level to 3000 feet in Venezuela, and from the arid deserts of the Guajira Peninsula and rain forests of Panama to the sawgrass-encompassed mahogany hammocks of the Florida Everglades. This involves a variety of mosquito vectors .Experimental studies demonstrated that many culicine mosquitoes were susceptible, with good vector potential, particularly those in the genera Culex and Aedes. Isolations of VEE virus have been made from Aedes scapularis, A. serratus, Psorophora confinnis (Venezuela); A. serratus. P. ferox, and Culex sp. (Trinidad); C. taeniops, C. vomerifer, C. pipiens (Panama); C. iolambus coronator (Mexico); and Culex (Melanoconion) sp. (Florida).
In contrast to wild birds, which have been defined as the vertebrate reservoir for mosquito infection with WEE, EEE, and SLE viruses, VEE virus appears to be dependent on wild rodents and possibly other small mammals for the vertebrate component of its natural cycle and epizootic dissemination. Experimental work with birds supports this observation of relative refractoriness to VEE virus. This would explain its restricted localization with periodic peripheral pulsations that, by mosquito vectors, spill the virus into human epidemics. This mechanism differs from the widely dispersed epidemic manifestations of the other three arboviral encephalitides.
Meteorologic or seasonal changes influence the dissemination of. virus from these foci. Epidemics have been observed to follow excessive rainfall, which amplifies the human- and equine-biting mosquito vectors: equine cases appear that usually manifest CXS signs, soon followed by occurrence of febrile illness in rural human residents of the same area.
When such dissemination happens on an epidemic scale, a high incidence of human infection occurs, often in a majority, immunizing the population so that an epidemic will not again be manifest until a sufficient number of new nonimmune persons are introduced into the region. This is thought to be the explanation of why human VEE in Venezuela was not observed for twenty years from 1942 to 1952. the remarkably high incidence in children reflecting, the non immune component of the total population.
Clinical Characteristics of Venezuelan Equine Encephalitis.
Onset following natural infection occurs after an incubation period of two to five days. A lapse from the time of infection as short as 24 hours has been reported following massive laboratory exposure to the virus or intimate contact of medical personnel with acutely ill infectious patients with virus recoverable from the nasopharynx.There is usually sudden occurrence of shaking chills, fever, and headache, which, rapidly becoming more severe, are accompanied by generalized malaise and aches and pains in specific regions. Sore throat is frequent, as are nasopharyngeal congestion and inflammation that may also be associated with other upper and lower respiratory symptoms and signs. Temperature often reaches 104° F., increased pulse and respiration rates reflecting the fever and upper respiratory involvement. Vomiting and diarrhea are frequent; signs of gastrointestinal bleeding have been observed.
The acute, influenza-like illness may last only 24 hours, or as long as four or more days. The longer the febrile period lasts, the longer the convalescence. A patient with a 24-hour illness may be fully recovered and back to work in a day or so, whereas an illness lasting several days may require several weeks for the patient to fully recover from the characteristic weakness and fatigue.
Blood examination frequently shows a severe leukopenia, with a relative lymphocytosis, although a mild leukocytosis may be observed. The earlier the blood count specimen is taken, the more likely a leukopenia will be detected. Because a blood specimen taken within the first 24 to 48 hours of illness will almost always yield virus, a sizable blood specimen for separation into serum should be collected at the earliest opportunity. Albuminuria will be detected in a minority of cases.Most patients suffer an intermittent or remittent fever, but biphasic cases have been observed in which, after’apparent recovery, another bout of high fever occurred. Any of these courses precedes the
occasional development of central nervous system signs that are first manifest by general depression of the sensorium. Progression to more severe involvement is marked by convulsions and coma. The rarity of nuchal rigidity is remarkable. The variety of peripheral neurologic signs of flaccid or spastic paralyses and changing reflexes is not distinguishably different from that of the other arboviral encephalitides.
Possibly because of the short incubation period, rapid onset, and fulminating nature of the CNS involvement, most patients have clear cerebrospinal fluid without abnormal numbers or types of cells and with no elevation of protein. In those in whom a pleocytosis is detected, the range is between 10 and 20 cells, chiefly lymphocytes.
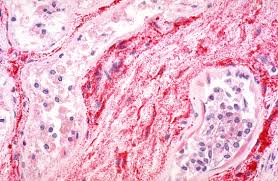
In the recent Venezuelan epidemic all fatalities were in children, Castillo reporting that most were between one and four years of age. Autopsies were performed on a number who showed the usual edema and hyperemia characteristic of arboviral encephalitis. In addition there was a remarkable amount of visible gross and perivascular hemorrhage in the brain and extensive pneumonitis, in some cases hemorrhagic. Detection of hemorrhagic lesions in the myocardium and tubular degeneration in some kidney tissues provided similarities to findings in characterized arboviral hemorrhagic fevers. Wenger reported the birth of congenitally defective hemorrhagic infants whose mothers had a history of an illness indistinguishable from VEE in the first or second trimester of pregnancy.
Epilepsy, flaccid and spastic paralyses, generalized tremors, insomnia, hallucinations, irritability, – and emotional instability have been observed months following discharge of children considered cured. Parkinsonism and epilepsy were observed in adults who suffered CNS complications during the infection.
Diagnosis
The clinical similarity to influenza makes distinctive clinical diagnosis difficult However, in the recognized range of VEE activity, following reports of an epizootic in equines, heavy rainfall producing an abundance of man-biting mosquitoes, the appearance of an epidemic of acute febrile disease in a rural population without commensurate cases in adjacent urban populations, and a low incidence but obvious occurrence of central nervous system complications strongly suggest the diagnosis of Venezuelan equine encephalitis viral infection. For many reasons it is essential to establish an etiologic diagnosis as soon as possible.
Virus can easily be isolated from the blood of an acutely febrile patient and from throat washings of the patient for an even longer period after onset;therefore, as soon as a diagnosis is suspected, collection of these specimens and immediate dispatch to the virus laboratory may establish a diagnosis soon enough for mosquito control measures to cause a dramatic and abrupt cessation of occurrence of new cases in humans.
Serologic diagnosis in cases seen too late for virus isolation, or to ‘ confirm the preliminary finding of VEE virus, is accomplished by demonstrating a fourfold rise or fall in CF and/or HI antibodies in two or more sequential serum specimens. Although there is accumulating evidence that there are antigenically detectable geographic differences in strains of VEE virus, some giving rise to two separate types (Mucambo and Pixuna of Brazilian Amazonia), the strains are similar and sensitive enough for any type to produce diagnostic antigen that in a serologic test will establish an etiologic diagnosis in a human case.
Venezuelan Equine Encephalitis Treatment.
There is no specific treatment, although considerable relief of discomfort can be accomplished by intelligent use of analgesics and antipyretics. Neurologic complications require appropriate nursing care, with maintenance of fluid and electrolytes to avoid further CNS damage. In such cases the temperature should be taken every one or two hours because of the possi-. bility of hyperthermia. If the temperature rises to 104° F., every external means to reduce it should be applied because loss of heat regulation may result in death.
Prophylaxis.
An experimental vaccine has been produced that is useful for protection of laboratory workers who must work with VEE virus. It is an attenuated live virus derived from an equine strain isolated in Trinidad. Reactions are frequent and severe enough to militate against general use of the vaccine for all but the most highly exposed, for whom the probability of accidental infection is great. There are several reports of VEE infection in vaccinated persons containing significant titers of neutralizing antibody against VEE virus; therefore, successful vaccination should not be considered an excuse not to continue exercise of intelligent preventive measures.
For rural residents of regions where recognized VEE virus is known to be prevalent, personal protection from mosquito bites through use of mosquito nets and screened windows at home and protective clothing outside is the most reasonable measure. This can be augmented by application of repellents to exposed skin surfaces, particularly after reports of epidemic or sporadic VEE cases in the region.
In a situation in which VEE cases are known to occur, it is important to establish the mosquito vector through special field studies. Subsequent mosquito control measures can then be intelligently planned for dealing with that particular vector. If an epidemic occurs before the identity of the vector species can be established, adjunct agents for mosquito control by fogging and residual spraying around human premises are essential.
Because of the frequency with which VEE virus has been recovered from the nasopharynx of patients and reports of medical personnel suffering the disease following intimate association with infected patients, isolation of the acutely ill and adherence to a medical regimen for isolation by medical personnel are strongly recommended.