Dural venous sinus thrombosis may occur in meningitis, may complicate epidural or sub dural abscesses, or may develop during the intracranial spread of infection from extracerebral veins. The thrombotic process may spread to connecting sinuses and cortical veins. Abscess formation within the thrombosed vessel may result in septicemia and infected emboli that travel to distant sites. The cavernous, lateral, and superior sagittal sinuses are most frequently involved.
Cavernous Sinus Thrombosis.
Infection can spread to. the cavernous sinus through venous channels by three routes: (1) from lesions of the upper half of the face through the facial veins communicating with the angular and superior ophthalmic veins, (2) from infections of the sphenoid and posterior ethmoid sinuses, inferiorly, and (3) from the ear, posteriorly. The initiating infection is usually an intranasal or facial furuncle, acute sinusitis, or an infection of the ear or mastoid. The widespread use of antimicrobial drugs in the treatment of superficial infections has markedly reduced the incidence of this disease. The majority of infections are due to Staphylococcus aureus, particularly in the presence of nasal furuncles.
Clinical Manifestations of Dural Venous Sinus Thrombosis.
The general clinical features are those of severe systemic infection: chills, fever, headache, nausea, lethargy, marked polymorphonuclear leukocytosis, and bacteremia. The specific findings are unilateral initially but become bilateral as the process extends to the opposite cavernous sinus via the connecting circular sinus. They include, in the case of infections about the face, unilateral edema of the forehead, eyelids, and base of the nose, as well as proptosis and chemosis — all due to obstruction of the ophthalmic vein as it enters the cavernous sinus. The Superficial veins over the forehead may be distended.
The retinal veins become engorged or even thrombosed. Retinal hemorrhages and papilledema occur but may be late manifestations. Involvement of the ophthalmic branch of the fifth nerve produces pain in the eye, photophobia, and hyperesthesia of the forehead. Partial or even complete paralysis of the ocular muscles develops as a result of involvement of the third, fourth, and sixth cranial nerves as they pass through the sinus. The pupils are usually dilated but may be small; the pupillary reactions are often lost.
In infection spreading by the inferior route (sphenoid sinusitis, etc.) the process may be less acute initially. A meningeal reaction commonly occurs, usually without organisms in the cerebrospinal fluid, but pyogenic meningitis sometimes occurs. Rarely, infarction and abscess of the pituitary complicate septic cavernous sinus thrombosis.
Differential diagnosis includes other causes of proptosis, especially orbital cellulitis, abscess, or acute carotid-cavernous fistula. Retinal hemorrhages, papilledema, and palsies of cranial nerves innervating extraocular muscles rather than general restriction of ocular movement from the mechanical effects of orbital swelling are useful differential points.
Lateral Sinus Thrombosis.
Thrombosis of the lateral sinus is almost always a complication of acute or chronic otitis media, mastoiditis, or of cholesteatoma formation. Rarely, infection may spread in a retrograde fashion from a focus in the neck or from a tonsillar abscess. StreptOcocci, predominantly group A, and staphylococci have been implicated most frequently. The clinical manifestations include chills, fever, and signs of increased intracranial pressure. Pain, venous engorgement, and edema behind the ear may result from associated involvement of the mastoid emissary vein and may extend into the neck over the jugular vein. Papilledema is common; it may be unilateral as a consequence of extension to the cavernous sinus on that side.
A generalized increase in intracranial pressure is more frequent with occlusions of the right lateral sinus, which is commonly larger and more important for venous drainage than the left. Convulsive seizures and obtundation occur, but focal neurologic findings are rare except when the thrombophlebitis extends into cortical veins over the convexity of the hemisphere. Rarely, ninth-, tenth- and eleventh- nerve palsies develop, presumably due to involvement of the jugular bulb and related venous channels.Cerebrospinal fluid pressure is elevated, and the fluid contains several to many hundred leukocytes (lymphocytes predominating) but no bacteria.
Superior Sagittal Sinus Thrombosis
The superior sagittal sinus is less commonly involved in septic thrombosis than are the lateral and cavernous sinuses. Infection may spread from the lateral or cavernous sinuses, from the pelvis by way of the vertebral veins, from a primary meningitis, or from a contiguous osteomyelitis and epidural infection. If thrombosis is restricted to that portion of the sinus anterior to the rolandic veins, and there is no associated involvement of cortical veins, then the process is usually asymptomatic.
Thrombosis of the posterior portion of the sinus results in increased intracranial pressure; at times there are engorgement of scalp veins and edema of the forehead. Extension of the inflammatory process into the cortical veins results in infarction of the underlying cortex. Focal seizures, which alternately involve one and then the other side of the body, are characteristic. Because the superior and mesial surfaces of the cerebral hemispheres are particularly liable to infarction, weakness and sensory changes are frequently more prominent in the legs. However, hemiparesis, homonymous hemianopia, aphasia, and paresis, or conjugate deviation of the eyes may occur.
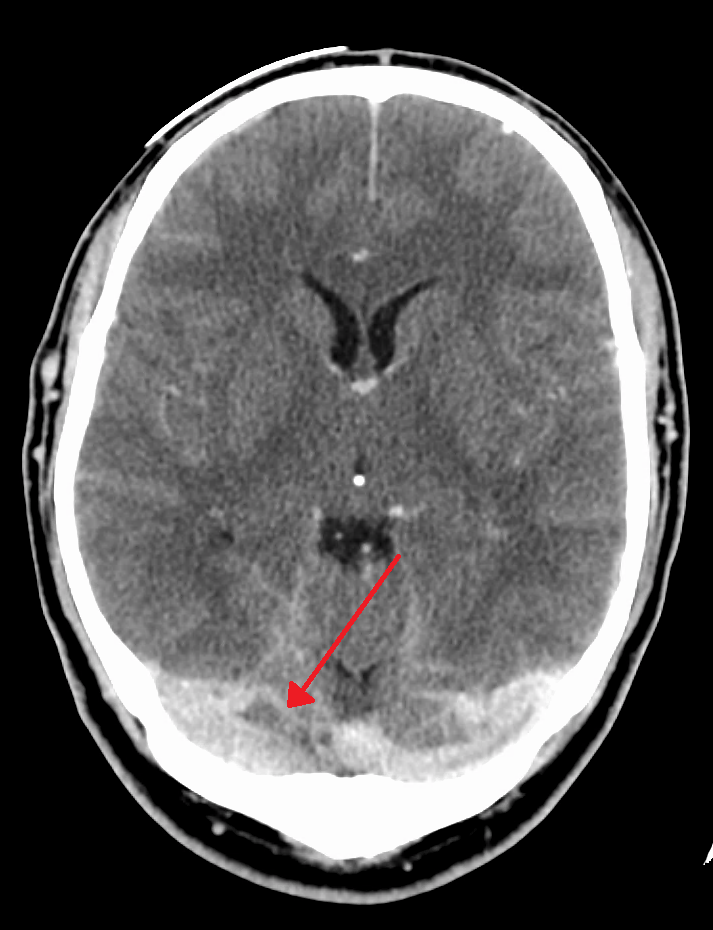
The cerebrospinal fluid findings are similar to those in lateral sinus thrombosis. A suspected diagnosis of major venous sinus thrombosis can often be confirmed by angiographic study.
Treatment Guidelines of Dural Venous Sinus Thrombosis.
Appropriate antimicrobial drugs in high dosage and surgical drainage, with removal of infected bone and extradural or intrasinus abscess, constitute proper treatment for major sinus thromboses. Ligation of the jugular vein in lateral sinus thrombosis to prevent spread of infected emboli is usually not necessary.
Because of the frequent involvement of penicillinase-producing staphylococci, the use of semisynthetic penicillins (nafcillin, oxacillin), cephalothin, or the combination of penicillin and methicillin is warranted until cultures are reported. Since infarction of cerebral tissue from venous thromboses tends to be hemorrhagic, anticoagulants are not employed. The prognosis for recovery is reasonably good when optimal treatment is given, although there are frequently residual neurologic symptoms and signs.
Dural venous sinus thrombosis is a rare but potentially life-threatening condition that requires immediate medical attention. If you experience persistent and severe headaches, visual changes, or other concerning symptoms, seek medical assistance promptly to receive a proper diagnosis and appropriate treatment. Remember, early intervention plays a crucial role in ensuring a positive outcome.