Amyotrophic lateral sclerosis (ALS) is also known as Lou Gehrig’s disease and motor neurone disease .This is a chronic progressive disease of the nervous system of unknown etiology. It is usually sporadic but rarely familial, and is characterized pathologically by degeneration of motor neurons in the spinal cord and the lower brainstem, and often of Betz cells in the motor cortex. Clinically, it appears in its usual form as a disturbance in motility, reflecting dysfunction of both lower and upper motor neurons.
Pathology.
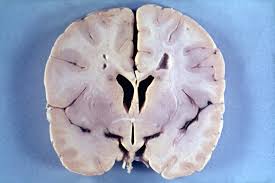
On gross inspection, the most obvious abnormality of the spinal cord is thinning of the ventral roots and reduction of the size of the cervical enlargement. In the brain, atrophy of the hypoglossal nerve and occasionally of the precentral gyrus is evident. Microscopically, there is a diffuse pallor of myelin staining, most noticeable in the lateral columns of the spinal cord, the bulbar pyramids, and the anterior limb of the internal capsule. Loss or degeneration of neurons occurs in the ventral horns and in the nuclei of some cranial nerves.
The motor nucleus of the trigeminal nerve and nuclei of the facial and hypoglossal nerves are particularly involved. Affected muscles show the typical features of neurogenic atrophy with intermingling of small, atrophic muscle fibers and fibers of normal size. The structure and staining of the affected fibers are preserved until late in the disease when they finally disappear, leaving residual clumps of hyper- chromatic sarcolemmal nuclei.
sclerosis is a disorder of later life with a peak incidence in the fifth and sixth decades. It is slightly more common in men than in women and is found in all races and on all continents. It has been estimated that in the United States there are about 3000 new cases occurring annually and a total of about 8000 to 10000 persons afflicted with the disease at any given time. The clinical picture of the disorder reflects the underlying pathologic changes of the lower and upper motor neurons.
Lower motor neuron dysfunction causes weakness and wasting of the afflicted muscles. An additional consequence of the disease process may be a spontaneous irregular discharge of motor neurons, reflected peripherally by irregular twitching in the distribution of one or several motor units. This is termed fasciculation. Fasciculations may be observed as continuous movements of portions of muscles anywhere in the body and may be perceived by the patient. Characteristically, fasciculations are widely distributed, extending beyond the territory of a single nerve root or peripheral nerve, and are ominous when associated with weakness.
Involvement of the upper motor neuron leads to spastic rigidity, augmented deep tendon reflexes, and extensor plantar responses. When the corticobulbar tracts are involved bilaterally, the syndrome of pseudobulbar palsy may ensue. In this state, voluntary swallowing, tongue movements, or facial mimicry may be impaired. In addition, the patient may have episodes of inappropriate crying or laughing which are often provoked by an innocuous stimulus and are dissociated from feelings of excessive sadness or mirth.
There are several clinical variations of the disease that depend upon the regional distribution and the relative involvement of lower and upper motor neurons. Most commonly the disease presents in the distal muscles of the upper limb. The anterior horn cells in the cervical region are the first affected, and this leads to the appearance of wasting and fasciculation in the upper limbs which is particularly obvious in the small muscles of the hand.
Involvement of both lateral and medial thenar groups leads to the thumb falling into the plane of the palm of the hand—the “simian hand.” Although bilaterally symmetrical in later stages, the disease may be unilateral or even hemiparetic early in its course. As the disease progresses proximal muscles and then muscles of the trunk and bulb become weak. In some cases involvement of motor units in the leg may be the earliest sign of the disease. The disease may present as foot drop, which is confused in its earliest stage with palsy of the lateral peroneal nerve. As the signs of lower motor neuron dysfunction are progressing, some associated signs of upper, motor neuron disease become evident, particularly in the lower extremities.
Less commonly, bulbar signs may predominate in the early stages of the disease, producing the syndrome of progressive bulbar palsy. The muscles of the palate, pharynx, and tongue are most commonly affected. Jaw movement and facial expression are impaired somewhat later. Extraocular movements are rarely involved in the disease. Involvement of the hypoglossal nucleus is an early sign, resulting in a slurring dysarthria and weakness of tongue movements. As the disease progresses, the tongue, small and shriveled, lies immobile but fasciculating in the floor of the mouth.
The palatal and pharyngeal musculature becomes weak, and aphagia, nasal speech, and regurgitation of liquids result. Later there is often wasting of the facial muscles, especially the orbicularis oris, which may be coupled with the signs of pseudobulbar palsy. Usually some signs of involvement of upper or lower motor neuron innervation of the trunk and limbs are evident in later stages of the disease.
Rarely, the disease may present as a progressive spastic paraparesis in which the evident signs of the disorder can be attributed to dysfunction of the upper motor neuron. This form of the disease has sometimes been called primary lateral sclerosis. At this stage it is not possible to make the diagnosis of amyotrophic lateral sclerosis, and full investigation, particularly to exclude spinal cord compression, is mandatory. If there is no evidence of denervation, it is probably not amyotrophic lateral sclerosis. Only the subsequent development—perhaps a number of years later —of fasciculations,. of electromyographic evidence of denervation, or of the characteristic pattern on muscle biopsy permits the proper diagnosis to be made with certainty. By then, the disease is no longer confined to the upper motor neuron.
Despite the massive involvement of upper and lower neurons of the cortical spinal system, there are no adventitious movements, signs of cerebellar dysfunction, sensory disturbances, or involvement of sphincteric function. In a few patients dementia may occur.
what causes Amyotrophic lateral sclerosis,You Must Know First Diagnosis of ASL.
In making the diagnosis of amyotrophic lateral sclerosis the only laboratory test of value is electromyography. A sampling of affected muscles will reveal a reduction in the number of motor units active on contraction, as well as fasciculations and fibrillation potentials which represent the electrophysiologic consequence of denervation. Nerve conduction velocities are normal until advanced stages of the disease. There are no characteristic changes in the blood chemistry or the cerebrospinal fluid. A muscle biopsy is useful in distinguishing between a neurogenic and myopathic process. However, the histologic findings in muscle are nonspecific for any neurogenic atrophy.
Differential Diagnosis.
Because of the bleak prognosis of amyotrophic lateral sclerosis, it is imperative that all efforts be made to establish with certainty the diagnosis of the disease. The disease can be diagnosed without difficulty when presenting in its most typical form as progressive, painless, diffuse muscle weakness with atrophy, fasciculations, and an associated spasticity, enhanced stretch reflexes, and extensor plantar responses. In the earlier stages, when presenting as a more localized disease, it is necessary to distinguish amyotrophic lateral sclerosis from other conditions which may produce lower motor neuron dysfunction, particularly when signs of corticospinal tract involvement are evident. When presenting as localized wasting of muscles, particularly in the hand, the disease must be distinguished from lesions of peripheral nerves.
Mononeuritis or multiple mononeuritis will have a distribution characteristic of the involved nerve or nerves, reduced or absent deep tendon reflexes, and sensory abnormalities in the territory of the sensory innervation of the nerve. The metabolic polyneuritides, such as diabetic polyneuritis, tend to involve the feet before the hands, and sensory abnormalities are common. Conduction velocity in those peripheral nerves that can be tested is commonly abnormal in these conditions. Polyneuritis of the Guillain-Barre variety will have a more rapid onset; it is unassociated with fasciculations and is usually accompanied by elevation of the cerebrospinal fluid protein. Compression of the brachial plexus by cervical rib may present itself with weakness and wasting of intrinsic muscles of the hand.
The relatively static and localized nature of the disease, the presence of pain, and confirmatory roentgenographic evidence of bony abnormalities will establish the diagnosis. Compression of cervical or lumbar nerve roots by osteoarthritic spurs or a herniated intravertebral disc may result in painless wasting, and in limb muscles is often associated with fasciculations. A differential diagnosis from amyotrophic lateral sclerosis in this condition may be further complicated by evidence of spasticity in the extremities, occurring as a result of extradural compression of the spinal cord by bony ridges of the vertebra.
Pain, sensory abnormalities, a fixed location of the defect, and localized EMG abnormalities, as well as the characteristic roentgenographic changes of the vertebral column, may help to establish this diagnosis. However, in some cases the differential diagnosis may be extremely difficult and may only be resolved by following the evolution of the disease.
Epidural compression of the spiral cord by tumor, by arachnoidal thickening secondary to syphilis or other infectious processes of the meninges, or in cervical spondylosis may lead to segmental weakness, atrophy, and long tract signs in the legs. Most such lesions cause bain, and the fixed nature of the lower motor neuron disorder and the evidence on myelography of a compressive lesion of the cord can usually establish the diagnosis. Intramedullary lesions of the spinal cord, including tumors or syringomyelia, usually interrupt segmental reflex arcs and also produce sensory signs. The sensory loss may occasionally be of the dissociated type with selective loss of pain sensation and preservation of touch and deep sensibilities over several segments.
When presenting as bulbar palsy, myasthenia gravis can be diagnosed by appropriate pharmacologic tests. The syndrome of primary lateral sclerosis is most commonly due not to amyotrophic lateral sclerosis, but to multiple sclerosis or spinal cord compression. Investigation of such a case must include careful cerebrospinal fluid examination and myelography. The diagnosis of motor neuron disease becomes established only when signs of lower motor neuron involvement are unequivocally demonstrated. Benign fasciculations or myokymia is a troublesome but innocuous syndrome of migrating or static fasciculations of skeletal muscles. It may be localized, often to one eyelid, or it can be more generalized.
It is common in younger patients. The distinguishing feature in the differential diagnosis is that weakness or wasting of muscles does not occur with benign fascinations. However, the overt fasciculations may alarm both the patient and unwary physicians, and may sometimes lead to a misguided clinical diagnosis of amyotrophic lateral sclerosis. However, such patients lack EMG evidence of muscle denervation. Degeneration of the lower motor neuron may occasionally occur as a remote effect of cancer on the nervous system, and is discussed under that topic.
Course and Prognosis.
Amyotrophic lateral sclerosis almost always has a dismal prognosis. In most cases death occurs within three to four years after the onset of symptoms. There are atypical cases in which the condition may appear to become arrested with little or no progression of symptoms over many years. In general the prognosis is worse when the initial symptoms are bulbar; survival in these cases seldom exceeds two years. Inability to handle secretions and weakness of the respiratory muscles are the predisposing causes of the usual terminal event, bronchopneumonia.
Treatment.
The absence of any treatment that could influence the course of motor neuron disease only increases the physician’s responsibility for the symptomatic care of these patients. In advanced cases tracheostomy, may be indicated to prevent the patient from drowning in his own secretions. Tube feeding or gastrostomy may prolong survival