Syringomyelia is a chronic disease of the spinal cord, characterized pathologically by cavitation of the spinal cord with gliosis and clinically by a mixture of segmental and supra- segmental motor and sensory abnormalities and trophic disturbances. When a syrinx occurs in the brainstem, the disease is called syringobulbia.
Etiology
The cause of syringomyelia is unknown. Several theories have been proposed to explain its pathogenesis, but none are entirely satisfactory. Because of the common association of syringomyelia with other congenital abnormalities of the neuraxis and skeleton, the most popular hypotheses have attributed the disease to developmental anomalies. One hypothesis has suggested that the disease is due to abnormal closure of the neural tube; another, that it results from the persistence of ependymal cell rests which later proliferate and cavitate. A third, proposed by Gardner, suggests that the cavitation is caused by distention of the central canal by ventricular fluid displaced caudally from the fourth ventricle as a consequence of atresia of the foramina of Luschka and Magendie.
The frequent association of intramedullary vascular malformations, vascular neoplasms, and gliomas with syrinxes has led Netsky to suggest that focal ischemia within the spinal cord caused by an abnormal vascular supply is pathogenic.
Pathology of Syringomyelia.
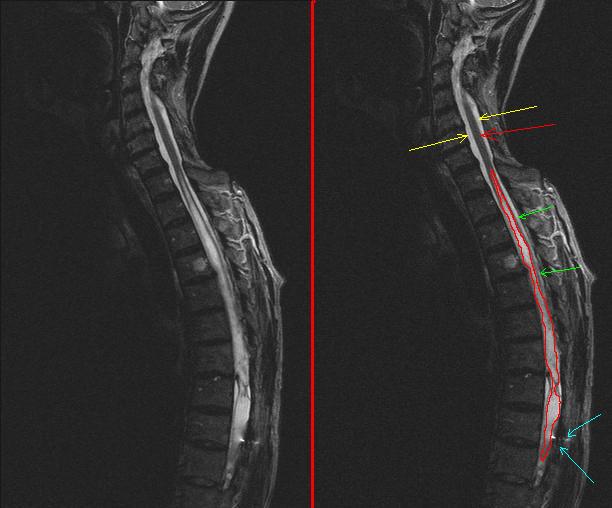
On gross inspection the spinal cord may appear normal, enlarged, or flattened in its anteroposterior axis, depending upon the size and state of the syrinx. The syrinx itself, when intact, is filled with clear, slightly yellow serous fluid. The. walls of the cavity are irregular, and consist of degenerate neural and neuroglial elements. The cavity usually surrounded by gliosis, composed for the most part of glial fibers. Abnormal blood vessels with hyalinized walls may sometimes be seen. There is usually secondary degeneration and demyelination of long ascending and descending tracts of the spinal cord and brainstem as a result of extension of the syrinx. The syrinx most commonly runs over several segments in the cervical cord.
It may extend into thoracic segments for a varying distance and may even terminate at lumbar levels. The cavity often begins in the gray matter adjacent to the central canal, and tends, as it enlarges, to interrupt the decussating fibers and destroy neurons in the dorsal and ventral horns. Within the thoracic cord, the cavity is commonly seen in the dorsal horns, and may affect the intermediolateral cell column, producing autonomic deficiencies. Syrinxes of the lumbar cord are uncommon.
Syringobulbia is associated with cavitation that is usually slitlike and often in communication with the fourth ventricle. Bulbar syrinxes commonly involve several cranial nerve nuclei, notably the descending root of the trigeminal nerve, and the solitary, ambiguous, and hypoglossal nuclei. They also may involve the medial longitudinal fasciculus, the pyramidal tract, and the medial lemniscus. Extensions into the pons are rare. A secondary syrinx consisting of central cavitation of the spinal cord and sometimes associated with gliosis may occur as a result of chronic arachnoiditis, spinal tuberculosis, or meningeal or vascular syphilis.
Syringomyelia Clinical Manifestations.
The clinical manifestations of syringomyelia depend upon the localization and size of the lesion. The disease most cqmmonly presents in the second decade, but sometimes the onset may be delayed until the patient is in his sixties or seventies. In its most usual form the signs and symptoms of the disease are referable to a syrinx in the cervical cord. The presenting symptoms often are wasting and weakness in the muscles of the upper extremity, associated with mild burning dysesthesias and loss of pain sensation distally in the arms. There are sometimes complaints of weakness of the legs, and bowel and bladder symptom. On examination the patient may have Horner’s syndrome as a consequence of interruption of the sympathetic pathways in the spinal cord. Nystagmus resulting from damage to the spinal projections of the medial longitudinal fasciculus may also be seen.
Muscle weakness in the upper extremity is usually associated with obvious atrophy, and frequently involves the small muscles of the hand. If the syrinx has extended into the corticospinal tract, weakness and spasticity in the lower extremities are evident. At the level of the lesion, the deep tendon reflexes may be absent or reduced. Because of the interruption of the second order afferent fibers arising from cells in the dorsal horn and crossing to the contralateral ventrolateral spinothalamic tracts, there may be a dissociated segmental type of sensory loss, often in a shawl or capelike distribution over the shoulders, upper trunk, and arms.
In this zone, light touch, vibration, and deep sensibility are preserved with a striking absence of pain and temperature sensation. When the lesion has extended to include the dorsal columns or the spinothalamic pathways, there are appropriate sensory abnormalities in the trunk and lower extremities. Trophic changes, particularly involving the hands, are common. Their pathogenesis is not known, but may in part be related to the absence of pain sensation and to. the interruption of vasomotor outflow to the limb. Unfelt burns from cigarettes or light bulbs may lead to tissue destruction and severe scarring. Cyanosis, hyperkeratosis, and thickening of subcutaneous tissues may result in puffy, swoller fingers. True hypertrophy of body parts may occur.
Traumatic osteoarthropathy (Charcot’s joint) is common. Sometimes the distal phalanges may atrophy and be lost painlessly, a condition, known as Morvan’s disease. The common clinical features of lumbosacral syrinxes are atrophic weakness of the lower limbs, loss of deep tendon reflexes, dissociated anesthesia, and fecal and urinary incontinence. If the lesion lies high in the lumbar cord, it may be associated with an extensor plantar response. Trophic changes of the lower extremity, particularly club foot deformities, are common. In syringobulbia the syrinx formation in the medulla may be unassociated with the syrinx in the cervical cord.
Common findings in this disorder are atrophy of the tongue, nystagmus, impairment of pain and temperature sensation on one side of the face, dysphonia, and respiratory stridor. In addition, sensory and spastic motor abnormalities of the extremities may be seen.There are many associated findings in syringomyelia. Papilledema may result from an associated hydrocephalus. Skeletal abnormalities are common and include cervical rib, spina bifida, premature closures of the skull, Klippel-Feil syndrome, basilar impression, and kyphoscoliosis. The association of syringomyelia with intramedullary gliomas or vascular tumors has long been recognized.
Diagnosis of Syringomyelia,Being A Doctor You Must Research
The diagnosis may often be made clinically by the observation of muscular atrophy and weakness, dissociated sensory loss, trophic changes, and long tract signs attributable to a lesion in the cervical cord. The laboratory findings in this disorder are nonspecific. The cerebrospinal fluid may be under increased pressure as a result of an associated hydrocephalus. A mild pleocytosis or increased protein in the cerebrospinal fluid may sometimes be seen. Electromyography may reveal evidence of denervation in affected muscles. Roentgenographic evidence of bony deformities may be helpful. Pantopaque x-ray myelography may sometimes giye evidence of a swollen syrinx.
Differential Diagnosis.
Syringomyelia must be differentiated from tumors of the spinal cord or cervical ribs, other bony anomalies, amyotrophic lateral sclerosis, multiple sclerosis, and tabes dorsalis. Intramedullary tumors of the cord, which produce comparable symptomatology because of a similar location, and extramedullary tumors, which can sometimes simulate an intramedullary lesion by compressing the anterior spinal artery, can often be differentiated from syringomyelia by myelography. Cervical rib may be identified roent- genographically, although the fact that this abnormality may be associated with a syrinx sometimes complicates the differential diagnosis.
Amyotrophic lateral sclerosis is never associated with sensory abnormalities. Multiple sclerosis can be differentiated by its remitting course and by the fact that muscular wasting, trophic changes, and dissociated sensory abnormalities are uncommon. Tabes dorsalis can be differentiated by the serology and by a different pattern of sensory loss.
Course and Prognosis.
The course of syringomyelia is variable, but is usually protracted over many years. In some patients there may be gradual deterioration; in others, changes may occur in a stepwise fashion. In some patients, after an initial attack, the disease may appear to have become arrested. In syringobulbia, death from respiratory paralysis may sometimes occur.
Treatment.
At present there is no satisfactory treatment for syringomyelia. X-irradiation or surgical decompression of the syrinx has been attempted in the past, but the therapeutic results have been at best doubtful.