Measles (rubeola) is an extremely contagious, febrile disease of high morbidity character.It is principally a benign disease of children, but may afflict with equal frequency persons of any age not previously attacked by its virus.
Etiology.
Measles is caused by a medium-sized RNA paramyxovirus approximately 1400 A. in diameter. The virus is thermolabile. having half-life of two hours at 37° C.; it is also inactivated rapidly below pH 4.5. Measles virus induces apparent infection with exanthem only in man and monkey. It has been found that tissue cultures derived from nonprimates, as well as from primates and chick embryos, will support propagation of the virus, as originally described by Enders and Peebles in 1954. The virus is structurally and biologically similar to the larger myxoviruses and agglutinates erythrocytes of the rhesus monkey and baboon in vitro and may thus be antiquated; inhibition of this reaction affords a method for tit-rating specific antibody in serum.
Prevalence and Epidemiology of Measles.
Measles is a disease of cosmopolitan distribution, endemic in all but isolated populations. It may occur at any time of the year, but most outbreaks are in the late winter and early spring, with a peak at the end of April. The disease recurs in epidemic cycles at two- to three-year intervals in most civilized communities that have been studied. This epidemic periodicity is best explained as a result of the introduction of new susceptibles into the population by birth or ingress from other areas. When the proportion of nonimmunes reaches a certain crucial concentration (45 to 50 per cent), disease and coincident dissemination of virus may occur to produce an epidemic.
It is likely that virus is introduced from sources external to the involved population, probably by incoming susceptible; there is no solid evidence of sub-clinical infection or a postinfection carrier state with unmodified measles to suggest local persistence of virus in interepidemic periods. Isolated communities such as the Faroe Islands (Panum) are infrequently attacked by measles, at which times manifest illness appears in virtually all persons not previously effected. In Greenland, a country not known to have been invaded previously by the disease, an epidemic resulted in overt measles in 99.9 per cent of the indigenous population (Christiansen and others).
Throughout most of the world, measles is a disease of children; most adults possess acquired immunity. Beyond the age of ten more than 90 per cent of the population have specific antibody. Although the peak attack rate coincides with the beginning of school (age six) in technologically advanced societies, it occurs between the ages of two and three in most underdeveloped countries. Morbidity and mortality rates do not appear to be influenced by sex or race. Case fatality rates are highest in children less than five years of age, and are also relatively high in the aged. Congenital infection has occurred.
There is no evidence that the virus may vary in virulence in nature. The oft-cited and notorious virulence of the disease in primitive, isolated, or crowded populations may be explained as a corollary of (1) more prevalent infection of feeble and aged adults, (2) poor environmental conditions, (3) inadequate medical care, and (4) secondary bacterial infections. A strikingly increased mortality rat£ is observed in areas such as West Africa in which protein-calorie malnutrition is prevalent.Because measles virus rarely induces fatal disease, it is evident that fatalities attributable to measles may vary in incidence according to the prevalence of bacterial pathogens and the resistance of the population to their presence.
Communicability.
Measles is one of the most contagious of infections. Demonstration of virus in nasopharyngeal secretions is in accord with epidemiological evidence that infection is disseminated and acquired by the respiratory tract. Close physical proximity or direct person-to- person contact is the usual requisite for infection.
Immunity of Measles.
An unmodified attack of measles usually confers lifelong immunity. This observation is in accord with the observed persistence of both complement-fixing and neutralizing antibodies after infection and the relatively high titer of antibodies present even in older persons. Able observers have described apparently authentic instances of second or even multiple infections. Definitive proof of recurrent infection with measles virus is lacking, however, because specific diagnostic laboratory tests have only recently become available.
Detailed study of a family subject to recurrent attacks suggests an hereditary defect in the capacity to develop immunity in certain cases. One such patient was found to be capable of antibody formation, and electroscopic analysis of the serum showed no deficit of gamma globulin. Temporary immunity may be passively acquired by receipt of convalescent serum or gamma globulin derived from the pooled serums of human adults (see Treatment). Humoral antibody is demonstrable in patients convalescent from measles modified by gamma globulin. The low incidence of measles in early infancy (first six months) is attributed to transient protection by placentally transferred maternal antibody.
Psychological or Pathological Response
Pathological changes in fatal measles usually represent the compound effect of viral and secondary bacterial infection. Pneumonia is almost invariably present; it is most frequently interstitial, but may produce purulent exudate within the alveolar. More representative are changes of the uncomplicated viral disease within the tonsillitis, nasopharyngeal, and appendices tissue removed during the promenade. These changes consist of sub-epithelial round cell infiltration and the presence of multifaceted giant cells.
The latter are so characteristic that skilled pathologists have predicted the development of rash from their presence in surgical specimens. Similar cells are commonly observed in tissue cultures infected with measles virus. Cytoplasmic and nuclear inclusions may be seen in epithelial cells. The lesions clinically apparent as Koplik’s spots derive from inflammatory mononuclear cell infiltration of buccal submucous glands and necrosis of focal vesicular lesions of the mucosa. Rash is the result of proliferation of capillary endothelial cells in the corium and the coincident exudation of serum, and occasionally erythrocytes, into the epidermis.No consistent or characteristic physiologic aberrations are observed with measles.
The transient hemoconcentration and albuminuria found with other febrile diseases may occur. A normal total leukocyte count or leukopenia is observed throughout the febrile period. Initially, the leukopenia is occasioned by a decline in lymphocytes on the first day of fever; subsequently, granulocytopenia ensues as well. The incubation period is characterized by neutrophilia, and convalescence by a relative lymphocytosis. Measles virus has been isolated from the leukocytic fraction of blood, and is propagable in suspensions of leukocytes in vitro. A false-positive serologic for syphilis may be observed.
Hormone-like Effects of Measles Infection. Several striking physiologic effects of measles, although poorly understood, mimic the influence of corticotrophin or the adrenal corticosteroids. These are transient suppression of the tuberculin reaction (observed also with measles vaccines), improvement in eczema and allergic asthma, delay in wound healing, and the induction of remissions in leukemia, Hodgkin’s disease, and lipoid nephrosis. Whether these effects are directly attributable to the virus or are hormonally mediated is not known.
Clinical Manifestations.
Following an incubation period that averages 11 days, measles becomes clinically manifest with symptoms of fever, malaise, myalgia, and headache. Within hours ocular symptoms of photophobia and burning pain are evidenced by conjunctiva injection, tearing, and exudate in the conjunctival sac. Concomitantly, or soon thereafter, catarrhal inflammation of the respiratory tract is manifested by sneezing, coughing, and nasal discharge. Less commonly, hoarseness and aphonia may reflect laryngeal involvement. In this prodromal stage of one to four days’ duration, petechial lesions of the palate and pharynx or tiny white spots on the buccaneer mucosa {Koplik’s spots) may herald the appearance of skin rash.
The white lesions described by Koplik characteristically occur lateral to the molar teeth, and typically are mounted on red areolae of injected mucosa, which may coalesce to form a diffuse red background. Not invariably present, they constitute a valuable, if not pathognomonic, diagnostic sign. The enan- them may involve other mucous membranes such as the vaginal lining. It may “overlap” the subsequent appearance of the cutaneous rash, by one to three days. Rarely, a transient, erythematous exanthema may occur in the prodromal period.
The rash of measles follows the prodromal symptoms by two to four days, occasionally as late as seven days. It first appears behind the ears or on the face as a blotchy erythema, spreads downward to cover the trunk, and finally is manifest on the extremities. The hands and feet may escape involvement. Initially, the eruption consists of discrete, reddish-brown macules that blanch with pressure. Subsequently, these lesions become slightly elevated, tend to coalesce, and may develop a hemorrhagic, nonblanching component.
Rash is sometimes very extensive in children with protein-calorie malnutrition, and skin lesions associated with kwashiorkor may develop at the site of the exanthem. The rash fades in the order of its appearance; its disappearance about five days after onset is attended by a fine, powdery desquamation that spares the hands and feet. At its maximum the exanthema usually marks the termination of malaise and fever in the uncomplicated illness.
The fever of measles is commonly of the typhoidal, progressively rising type, and falls by lysis. It persists for about six days, and frequently reaches 103° F. In the adult, fever may follow rather than antedate the catarrhal symptoms. Throughout the febrile period, productive cough and auscultatory evidence of bronchiolitis may be
evident. These manifestations may persist after defervescence, and cough is often the last symptom to disappear. It is probable that bronchopulmonary symptomatology is an integral part of the primary viral infection; roentgenographic evidence of pulmonary involvement is frequently seen in the uncomplicated disease in the absence of leukocytosis and obvious bacterial infection.
Complications.
It is difficult to distinguish between those complications directly attributable to the virus of measles and those resulting from secondary bacterial infections. The persistence or recurrence of fever and the occurrence of leukocytosis are presumptive evidence of the usual bacterial sequelae of otitis media or pneumonia. The pneumonia resembles other forms of viral pneumonia and is often caused solely by a specific reaction to the measles virus. Superimposed bacterial infection is common, however, and accounts for most of the severe or fatal cases. Pneumococcus, Streptococcus hemolyticus, Staphylococcus aureus, and Haemophilus influenzae are the usual secondary invaders. The incidence of bacterial complications is increased by crowding, debility, and the prevalence of bacterial pathogens in the population. Bacterially engendered sequelae may be unduly frequent in crowded contagious disease hospitals.
Serious complications directly related to the measles virus are rare. Laryngitis of sufficient severity to embarrass respiration has been observed, and may warrant tracheostomy. Electrocardiographic abnormalities may be found in as many as 30 per cent of children, but clinical evidence of cardiac disease is meager in such cases. Abdominal pain or diarrhea may be related to invasion of lymphoid tissue of the appendix or Peyer’s patches. These symptoms may lead to unnecessary surgery before‘the appearance of the typical rash. The frequency of stomatitis and gastrointestinal symptoms is greater in malnourished children in tropical areas and may reflect coincident bacterial and parasitic infection.
Encephalomyelitis.
A rare (0.01 to 0.5 percent) but serious consequence of measles is a demyelinating encephalomyelitis that may appear from one to fourteen days after the onset of infection. This complication is associated with a recurrence of fever, and headache, vomiting, and stiff neck. Stupor and convulsions occasionally follow. Localizing neurologic symptoms may or may not be present. Death ensues in about 10 per cent of patients; about half of survivors suffer permanent residuals of varying severity. Recently, abnormal electroencephalograms were recorded in 51 per cent of children with measles without evidence of encephalitis. In some of the children the abnormal encephalographic findings were persistent. The presence of a measles-like virus has been demonstrated in patients with subacute sclerosing panencephalitis.
Diagnosis of Measles.
The experienced layman can diagnose typical measles. The querulous, bleary- eyed child, his face blotched and his nose crusted with exudate, presents a characteristic, if miserable, picture as he breathes open-mouthed between paroxysms of sneezing and coughing. The severity of the catarrhal symptoms distinguishes the disease from other eruptive fevers. In the prodromal period the diagnosis should be suggested by (1) fever higher than that of the usual common cold, (2) known measles in the community, and (3) Koplik’s spots on the buccal mucosa.
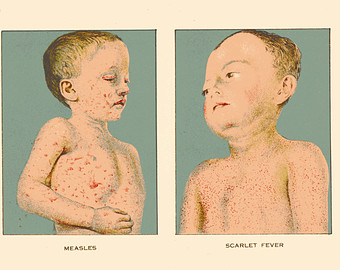
Differential diagnosis (see accompanying table) includes consideration of rubella, scarlet fever, exanthema subitum, infectious mononucleosis, secondary syphilis, drug eruptions, and infection with certain Coxsackie and echoviruses. Of value in excluding these possibilities are the milder course and pinker rash of rubella, the sore throat and leukocytosis of scarlet fever, and serologic tests for infectious mononucleosis and syphilis.The rash of exanthema subitum does not appear until the termination of fever. Fever, enanthema. and catarrh are uncommon with the cutaneous manifestations of drug hypersensitivity.
Specific Diagnosis of Measles.
Specific diagnosis depends on the isolation of measles virus from throat washing, blood, or urine by inoculation of various types of tissue culture with materials obtained during the first five days of illness. Increase in specific antibody may be detected as early as the first or second day of rash by the complement- fixation test. Antibody is also demonstrable by neutralization and hem-agglutination-inhibition procedures.Presumptive diagnosis may be made if giant cells are detected in stained smears of nasal exudation in the preeruptive period.
Prognosis.
Uncomplicated measles is rarely fatal, and complete recovery from the disease is the rule. Fatalities are almost always the result of secondary streptococcal or pneumococcal pneumonia, occurring principally in children below the age of five who become infected after the dissipation of passive neonatal immunity. Mortality in underdeveloped countries may be 250 times that observed in the United States or northern Europe. Case fatality rates are also high in elderly and tuberculous patients. Congestive cardiac failure is a common cause of death in patients over 50 years old.
Antimicrobial drugs effective against the usual secondary invaders have reduced the case fatality rate of measles sharply. The incidence of otitis media and pneumonia may be lowered by the prophylactic use of penicillin or a tetracycline early in illness.Encephalitis occurs as frequently in mild as in severe measles. However, modification of measles by gamma, globulin prophylaxis (vide infra) affords an improved prognosis with reference to the encephalitic complication.
Treatment.
There is no specific treatment for measles.But here is some trements of measels
Symptomatic Therapy.
In the absence of complications, bed rest is the essence of treatment in this usually benign, seiflimjted disease. Codeine sulfate (0.015 to 0.06 gram) is useful in the amelioration of headache and myalgia and is effective in the management of cough. Aspirin (0.3 to 0.6 gram) may be employed for its analgesic and antipyretic actions. Diet should be unrestricted. Bright light is not an ocular hazard, but photophobia may require darkening of the patient’s room.
Antimicrobial Prophylaxis.
The course of uncomplicated measles is not influenced by antimicrobial therapy. In common practice the incidence of serious bacterial infections is not sufficient to justify the routine prophylactic use of antimicrobials. Certain special circumstances may- warrant full therapeutic dosage with penicillin or the tetracyclines in anticipation of the poteintially fatal sequelae of pneumococcal or beta hemolytic streptococcal infections. These circumstances include treatment of the chronically ill the very young, or the aged, and the treatment of patients under crowded conditions that foster the increase and dissemination of pathogenic bacteria, as may occur in contagious disease hospitals. If careful observation of the patient is possible, rational therapy is based on the prompt recognition and etiologic definition of complications, followed by initiation of the appropriate antimicrobial drug in proper dosage.
Prevention.
The administration of convalescent serum or gamma globulin during the period of incubation may prevent or modify the manifestations of illness. The degree of modification obtained is dependent upon the quantity of antibody given and the time of its administration. In children of less than six years, the intramuscular injection of 0.025 ml. of gamma globulin per pound in the first half of the incubation period results in disease of lessened severity. Two to four times this amount will prevent disease in nearly 80 per cent of children. In older children and adults, one and one-half to two times as much globulin is recommended. In young or debilitated children the aim is complete prevention of disease. In children over five, less subject to complications, the goal of prophylaxis is attenuation of the infection sufficient to lessen symptoms but no: the development of effective immunity.