Autonomic Failure is an uncommon disorder first clearly described by Bradbury and Eggleston in 1925 as idiopathic orthostatic hypotension; it has been more recently emphasized as including more generalized autonomic and nervous system defects. The cause is unknown and the course progressive, disability or death usually occurring within five to ten years after onset.
Pathology and Pathogenesis.
Only a limited number of patients have received detailed examination of the central and peripheral nervous system at autopsy, not always with consistent findings. Degenerative changes have been found involving the autonomic ganglia, the intermediolateral and ventral neurons of the spinal cord, as well as various nuclear structures in the brainstem, the cerebellum, and the basal ganglia. However in some patients with apparently typical clinical disease, any or all of these structures have also been found to be histologically normal, leading to the hypothesis that a defect in autonomic transmitter function precedes any morphological changes.
Suggestions that the neuropathologic changes are anoxic and secondary to recurrent hypotension are unlikely to be correct, since the lesions lack the appearance and distribution of those caused by well documented anoxia.
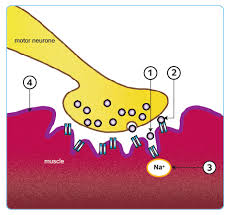
Several observations support the idea of a defect in transmitter function. Most of the patients demonstrate a blood pressure hypersensitivity to injected levarterenol, implying the absence of the humoral agent in the sympathetic ganglia. Also, patients with neurogenic orthostatic hypotension have been found not to synthesize norepinephrine and its metabolic products in normal amounts and to have below normal urinary catecholamine levels. Since the drug tyramine, which acts to release norepinephrine from peripheral autonomic nerve terminals, is effective in elevating the blood pressure, at least some epinephrine synthesis must be going on in postganglionic peripheral nerve terminals, but whether this is of a normal or reduced amount is unknown.
Clinical Manifestations.
Symptoms of autonomic insufficiency predominate initially. These include impotence in males, consti nation, heat intolerance with anhidrosis, and above all, weakness or faintness on rising to an erect position or during quiet standing. Urinary urgency or retention is common. As the disease progresses, symptoms of more
generalized neurologic dysfunction appear. Some patients develop a Parkinson-like illness with hypokinesia, rhythmic postural tremor, and mild to moderate rigidity. Others develop a cerebellar type of incoordination plus a gross rhythmic tremor in the lower extremities. The mind remains clear.
Physical signs include prominent evidence of autonomic insufficiency. Pupillary abnormalities with Horner’s syndrome can alternate from side to side. Even with-a high environmental temperature there is diffuse anhidrosis of the trunk and extremities. The blood pressure is normal when the subject lies supine, but when he stands, systolic and diastolic pressures drop 20 to 40 mm.
Hg or more but the pulse fails to accelerate. In the early stage of illness the blood pressure can gradually elimi during continued standing, but as the disease advances, autonomic compensation decreases then fails altogether, and syncope with unobtainable blood pressure tends to interrupt any sustained effort’ to -be erect. By this time, many patients Have associated signs of generalized neurologic dysfunction, including the Parkinson- like signs mentioned above as well as a cerebellar type of incoordination, muscle wasting and fasciculations, coarse tremors, and extensor plantar responses. Signs of peripheral’ neuropathy are notably lacking in the idiopathic disease.
Laboratory tests of the usual type are valueless except to exclude other disorders, but confirmation of the autonomic insufficiency makes the diagnosis.
Birchfield has presented a useful approach to evaluating autonomic insufficiency. Briefly, the evaluation investigates the blood pressure response to tilting and quiet standing, the patient’s ability to sweat when heated, a cold pressor test (the response is absent), the blood pressure response to injected levarterenol and sublingual nitroglycerin (the responses are hyperactive), and the response to the Valsalva maneuver (the normal blood pressure overshoot with its accompanying tachycardia fail to occur)
Differential Diagnosis of Autonomic Failure
Orthostatic hypotension can accompany acute cardiac failure (as with myocardial infarction or severe aortic stenosis), blood volume depletion (as with gastrointestinal or other massive hemorrhage), or vasodepressor syncope, but in all these conditions other signs of autonomic activity such as tachycardia and sweating are present and signs of diffuse neurologic illness are absent.
Autonomic insufficiency also accompanies some clearly identifiable neurologic diseases, including central thiamine deficiency (Wernicke’s encephalopathy), tabes dorsalis, syringomyelia, surgical sympathectomy, the neuropathies of diabetes, amyloidosis, and the Guillain-Barre syndrome, and a small fraction of patients who have vascular occlusive disease producing infarction or ischemia of brain stem autonomic centers. The differentiation from most of these illnesses is readily made by the typical signs, symptoms, and laboratory findings of each, and particularly by the fact that most of them produce sensory impairments in the extremities and other peripheral nerve abnormalities which are altogether lacking in idiopathic autonomic insufficiency.
Course and Treatment.
Although treatment is rarely completely satisfactory and does not affect the disease itself, much can be done to help these patients symptomatically, particularly during the early phase of the illness. Nine-a-fluoro- hydrocortisone given regularly by mouth is often effective in counteracting the orthostatic hypotension; it presumably operates ‘partly by increasing the blood volume. Elastic bandages on the legs may help by reducing venous pooling. Placing the head of the bed on six-inch blocks for sleeping has been found to lessen the next day’s degree of orthostatic hypotension.
Pressor agents have generally been useless because of their short, intense action and undesirable side effects. However, a combination of monoamine oxidase inhibitors (which prevent the breakdown of tyramine in the liver) and tyramine (which in the United States must presently be given in the form of New York State .cheddar cheese, since the drug is not approved by the United States Food and Drug Administration) has been found effective in maintaining the erect blood pressure of some patients previously bedridden from their illness.