Serum sickness is a disease characterized by fever, arthralgia, skin eruptions, and edema which appears alter injection of a foreign serum or serum proteins and is dependent upon an immune response of the patient to the injected serum. Hypersensitivity reactions to a variety of drugs may produce an identical illnes* Etiology. With the advent of antimicrobial therapy, the use of serum for the treatment of microbial diseases has declined markedly; the moat common cause for “serum sickness” at present is not serum itself but exogenously administered drugs, particularly the antimicrobials. Serum therapy is still used primarily for the neutralization of bacterial toxins such as tetanus and botulinus toxins and also in the form of rabies antiserum.
The incidence and severity of the diwaw are clearly related to the type of serum preparation as well as to the amount administered. Of patients given prophylactic tetanus antitoxin prepared in horses, approximately 2 to 6 per cent will develop symptoms of serum sickness. The figure is considerably higher for three patients receiving equine rabies antiserum; approximately 16 per cent of these patients develop serum sickness. In general, there is an increasing incidence and severity through childhood, adolescence, and adulthood. Reactions in children are quite mild, lasting from one to four days, whereas in patients over the age of 15. the disease is more frequent and more severe.
Different methods of production of various equine antisera may have a profound effect upon the serum sickness liability of the product Most tetanus antitoxin preparations involve a peptic digestion which does not impair antitoxic properties while hydrolyzing many of the proteins present in the serum. In contrast, antirabies antiserum is not subjected to peptic digestion because of the great loss of antibody encountered with the enzymatic treatment. The most important factor concerned with the development of serum sickness is the total amount of serum administered. Recommended doses of tetanus antitoxin and rabies antisera vary considerably from time to time; from 5 to 10 ml of tetanus untitoxin may product* serum sickness in 5 to 10 per cent of patients, whereas80 ml will almost always result in illness. Age and dose relationships in serum sickness resulting from drugs arc not as clear cut as with serum or serum proteins In most cases the drug by itself is not capable of inducing the disease and must combine with a protein of the patient to form a complete antigen or immunogen In such a situation the genetic potential of the patient of forming complete antigens and producing antibodies to them must be considered in addition to the patient’s age and the dose and duration of the drug given.
Serum Sickness Mechanism.
The essential basis of serum (ickntu in antigen-ant ihody interaction. A blood level of circulating foreign protein can he measured in patients shortly after beginning serum treatment. In the early stages the administered protein is cataholized in a manner similar to that seen in the animal from which it came. This is the latent period and usually lasts from four to ten days, during which time the patient develops an immune response that is evidenced by the appearance of antibody directed against the injected protein. As soon as antibody ap-pears, it combines with circulating foreign protein un-tigen to form soluble complexes. These complexes have a varied fate, depending upon their nature and the ratio of antigen to antibody in the complex.
Experimental studies. in the rabbit primarily, have shown a deposition of antigen-antibody complexes beneath the endothelium of blood vessels and within the basement membrane of these vessels. Complexes containing antibodies of the IgM or the IgG classes may initiate fixation and activation of the complement sequence. With localization of complement-containing complexes in the walls of blood vessels, polymorphonuclear leukocytes an* attracted to the site and appear to injure the vessel by release of potent enzymes found in their lysosomal granules. The vascular injury mediated by complement and polymorphonuclear leukocytes may lead to thrombosis and hemorrhage. typified by the petechial or ecchymotic rash attendant on serum sickness.
Another manifestation of the interaction of antigen and antibody is the release of potent vasoactive materials such as histamine, serotonin, bradykinin. and slow-reacting substance (SRSAi. all of which lead to vasodilatation and leakage of protein and fluid from the vascular space into the tissues, resulting in edema. The disease vanes from species to species in laboratory animals. As most of the work has been done in the rabbit, it is pertinent to note that the renal disease, which is a frequent and important aspect of immune complex disease in the rabbit, is often nonexistent or a very mild component in the usual human patient.
Continuation of disease is dependent upon a continual supply of anti Ren Removal by the reticuloendothelial system of the immune complexes is signified by a rise in serum antibody directed against the foreign proteins, and reduction of symptoms and signs of illness. Unless the foreign proteins are readministered, the disease is self-limited. During convalescence and for long periods thereafter, antibodies against the foreign proteins are readily demonstrable in the patient’s serum. Readmims-tration of foreign antigen promptly leads to formation of immune complexes and clinical manifestations of disease. which continue until antigen is entirely removed from the circulation.
Clinical Manifestations of Serum Sickness
The onset of disease is often heralded by itching and discomfort, frequently at the site of serum injection Fully developed serum sickness is a miserable disease The unfortunate patient lies on his side in bed with a swollen, distorted face, often resulting in closure of both eyes so that he cannot sec, with a skin itching all over and often covered with an urticarial or erythematous rash He is reluctant to scratch his skin hecauv of the pain in all his muscles and joinls upon movement, and so he lies quietly in lx*d suffering from headache, itching, and joint pmn Especially frightening and discomforting is the appearance of neurologic manifestations which may result in weakness of an extremity or a sensory deficit, or occasionally an isolulcd facial palsy. Compounding the patient’s difficulties may be abdominal pain, nausea, and vomiting. Upon examination a generalized lymphadenopathy may be palpated, especially prominent in the regions draining the site of injection of the serum At that site there may be a local rash with erythema and either urticaria or tenderness, and this may provide a potent clue for the physician as to the nature of the illness. Occasionally, auscultation of the chest reveals a cardiac arrhythmia or a pericardial friction rub. The spleen is usually not palpable.
A common manifestation is fever of 38.3 to 39“C (101 to 102 Ft. and. in addition to the subjective complaints of joint pain, the patient may manifest objective arthritis with swelling, redness. and accumulation of fluid in joints The skin may show a petechial or purpuric rash in addition to the more common urticarial eruption.
laboratory Studio Examination of the blood may reveal a mild leukocytosis, and circulating plasma cells have been observed The sedimentation rate is usually normal or only slightly elevated. Eosinophilia occurs, but is relatively uncommon The urine may show slight proteinuria, a few red cells, and occasionally a few cast?. but there are rarely significant evidences of renal impairment.
Examination of the serum proteins of the patient reveals circulating horse gamma globulins and macroglobuhns present early in the disease, and predominantly anti-hor.-e IgA globulin antibodies late in the disease and during convalescence. The development of antibodies to horse alpha-2-macroglobulin in the sera of patients recovering from serum sickness suggests that this component of the equine serum which lacks any antibody value could be deleted in manufacture without impairing the antitoxic benefits of the serum. Serum complement levels are reduced for variable periods dur ing the di.MMM? and then return to normal.
Treatment and Prognosis of Serum Sickness
Very mild Symptom* of pruritus and skin rash may be controlled by an antihis tamine. such as brompheniramine, 4 mg given every four hours Epinephrine and sympathomimetic amines have been recommended in the past for the treatment of the urticaria of serum sickness, and salicylates for the treatment of joint pains. However, for all but the mildest symptoms, adrenocortical steroids in the form of prednisone can be given with great safety and efficacy, and the patient need not suffer with less effective medications. As this is a self-limited disease with a natural course of one to three weeks, the usual hazards of steroid therapy are not realized before treatment is stopped A treatment course of 40 mg per day for four or five days may be sufficient, even for quite severe disease Symptomatic improvement appeurs often within hours of the onset of steroid therapy and sometimes is remarkable within 24 hount Prevention Tetanus antitoxin prepared from human serum i# now commercially available in many parts of the world When this is available, there is no reason to choose horse serum to obtain antitoxic benefits When equine sera must be used in treatment, patients -hould be carefully questioned concerning prior exposure and for allergic symptoms to other horse products, such as horse dander or horsehair, as found in horsehair mattresses.
All patients, regardless of history, should be skin tested by production of a minimal wheal (0.01 to 0.02 ml i of a 1:10 dilution of the serum to be tested After 15 to 20 minutes the skin site is examined for an urticarial wheal, and in its absence treatment may be instituted If the patient is allergic and the necessity for serum treatment is great, desensitization may be attempted by repeatedly injecting small amounts of serum beginning in diluliomt of 1 100 and doubling the tolerated amount about every 15 or 20 minutes until the appropriate dose is achieved.
Such treatment is hazardous because of po* sible anaphylaxis, and the indications for it should be scrutinized carefully.In patients who have developed serum sickness after tetanus antitoxin, active immunization should be begun during the patient’s convalescence from serum sickness.
It is generally advisable to immunize agam<t tetanus all individuals who are seen by the physician in connection with unrelated ullergic disease and found to be sensitive to horse dander or horse products The immunization can be accomplished by use of tetanus toxoid Occasionally, in the course of serum therapy a/i ucute anaphylactic reaction occurs, consisting of sudden vascular collapse, aevere pruritus of the face, hands, and feet, often accompanied by bronchospasm and incontinence of stool and urine.
Such events must be treated promptly uith epinephrine and not adrenocortical steroids A tourniquet should he placed proximal to the injection site of the drug or serum, and 0.2 ml of epinephrine injected into the site of injection which will slow absorption from the site. An additional 0.3 to 0.5 ml of 1:1000 aqueous solution of epinephrine should be given subcutaneously above the tourniquet if the patient has an effective blood pressure.
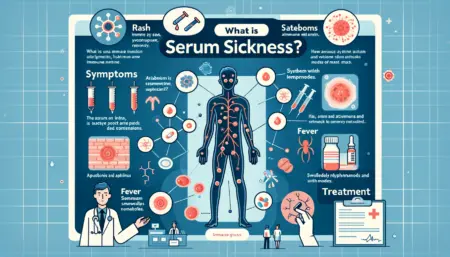
Serum Sickness is an immune response that occurs as a reaction to certain medications or antiserums. It’s a type of delayed hypersensitivity reaction. Here’s a tabular overview of how it works:
| Aspect | Details |
|---|---|
| Cause | Reaction to foreign proteins in antiserums or certain medications. |
| Pathogenesis | Immune system forms immune complexes with these foreign proteins. |
| Immune Response | Type III hypersensitivity reaction. |
| Onset | Usually 7-10 days after exposure to the triggering substance. |
| Symptoms | Fever, rash, joint pain, swelling, lymphadenopathy, and sometimes kidney damage. |
| Diagnosis | Based on clinical history and symptoms; laboratory tests may help. |
| Treatment | Discontinue the offending agent; symptomatic treatment with antihistamines, corticosteroids, and sometimes analgesics. |
This table offers a succinct overview, but the specifics can vary based on individual cases and the exact triggering substance.
Conclusion
Now that you have gained a better understanding of serum sickness, its symptoms, causes, and available treatment options, you can approach your health decisions with confidence. Remember to seek medical attention if you suspect serum sickness and take precautionary measures to minimize the risk of exposure. With this knowledge, you can prioritize your health and well-being effectively.
