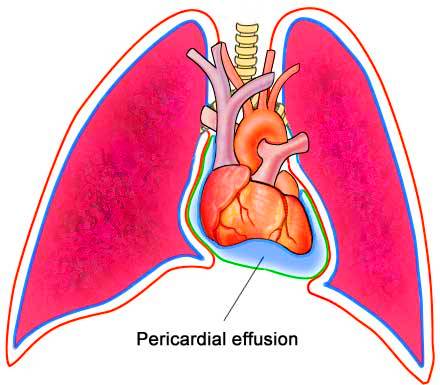
The pericardial Effusion consists of the accumulation of fluid, which can be plasma or blood in the membrane that surrounds the heart, and can cause a cardiac tamponade that is a serious situation that can lead to death. It may be the first sign of acute pericarditis, and its severe hemodynamic consequences may actually obscure the classic signs of the underlying pericarditis. Although chronic pericardial effusion may be accompanied by a pericardial rub, the insidious development of this condition without other evidence of pericardial involvement may simulate progressive heart failure and, unless readily recognized, may lead to death, even though it is an easily treatable condition.
An understanding of the pathophysiology of pericardial effusion and tamponade makes the physical findings of this disorder more obvious and understandable. The circulatory effects of pericardial effusion and tamponade are directly related to the rate at which the effusion develops. The sudden development of a pericardial effusion of several hundred milliliters of fluid may provoke profound hemodynamic changes, whereas the more gradual development of pericardial effusion may be almost asymptomatic despite accumulations of several liters of fluid.
Cause of pericardial effusion
The cause of the pericardial effusion is often related to pericarditis because the effusion is usually a consequence of this inflammation in the membranes of the heart.Some causes that can lead to this inflammation are:
- Bacterial, viral or fungal infections;
- Autoimmune diseases such as rheumatoid arthritis or lupus;
- Accumulation of urea in the blood as a consequence of renal insufficiency;
- Hypothyroidism;
- Metastases of lung, breast, or leukemia cancer;
- Cancer in the heart;
- Heart injury or trauma;
- Acute myocardial infarction;
- Medications for high blood pressure such as hydralazine.
The primary’ cause for the clinical and hemodynamic signs of pencardial effusion and tamponade is the accumulation signs or pencaraiai enusion ana lamponuue is tne accumulation of fluid in the pericardium sufficient to prevent adequate filling of the cardiac chambers. Since venous inflow to the heart is markedly decreased, there is accumulation of blood in the venous system that is reflected in marked jugular venous distention and hepatic engorgement. If the process is chronic, there is usually peripheral edema as well, jugular venous distention is usually unchanged or decreased by deep inspiration. The striking increase in jugular venous distention with inspiration (Kussmaul’s sign), which is frequently seen in constrictive pericarditis, is rarely seen in pericardial effusion because the expected increase in venous inflow into the right heart during inspiration is still preserved.
CARDIAC TAMPONADE And Pericardial Effusion
The most severe complication of a pericardial effusion, no matter what its cause, is the development of cardiac tamponade. Cardiac tamponade is a classic example of the vicious circle process in medicine. Accumulation of fluid in the relatively nondistensible pericardium initially limits cardiac filling and therefore cardiac output. As cardiac output declines, artenal pressure and coronary’ artery filling decrease. Coronary flow and thus mvocardial function are further compromised by tachycardia and external pressure on the superficially lying coronary arteries. Eventually this decline in cardiac filling, decrease in cardiac output, fall in arterial and coronary artery filling pressure, and decreased coronary flow lead to severe myocardial ischemia, which initiates an even greater decline in myocardial function. Unless this cycle of events is contravened by elimination of the effusion, a fatal outcome is certain.
Symptoms of pericardial Effusion
The symptoms of pericardial effusion vary according to the severity of the disease and the amount of fluid accumulated in the pericardial space, which can be:
- Difficulty breathing;
- Worsening of tiredness when lying down;
- Pain in the chest, usually behind the sternum or on the left side of the chest;
- Cough;
- Low fever;
- Increased heart rate.
Diagnosis of pericardial effusion may be made through physical examination through cardiac auscultation, observation of symptoms, and may be confirmed by examination such as chest x-ray, electrocardiogram, or echocardiogram.
TREATMENT OF Pericardial Effusion
The ultimate proof of the diagnosis of pericardial effusion and also an often mandatory’ procedure to provide relief from cardiac tamponade is pericardiocentesis. This is accomplished by inserting a medium-sized needle high in the epigastrium in the angle formed between the left border of the xiphoid process and the lower left rib cage. After suitable local anesthesia, the exploring metal needle is connected by an insulated wire to the V lead electrode of the FCG. The needle is slowly advanced upward and slightly posterior in a line toward the medial third of the right clavicle. While the needle is being advanced, the electrocardiogram should be continuously monitored. Contact with the epicar-dium will be signaled by the development of marked S-T segment elevation on the ECG record.
This procedure not only helps prevent puncture of the heart but also provides confidence that one has not perforated the heart if a frankly bloody pericardial effusion is encountered. In acute cases of tamponade such as can occur with aortic dissection or cardiac trauma, it may be impossible to ascertain whether one is draining the pericardial space or actually removing blood directly from a cardiac chamber. This quandary can usually be eliminated by making certain that there has been no evidence of a current of injury on the recorded V lead of the ECG. Once fluid is obtained by aspiration, it should be examined microscopically for the number and type of cells present and the presence of bacteria. The fluid should also undergo cytologic examination, be submitted for bacterial and tuberculous culture, and be analyzed for sugar and protein content, as well as LDH enzyme and rheumatoid factor if clinically indicated.