Lung Abscess is the death of lung tissue caused by microbial infection, characterized by the formation of cavities ranging from a few millimeters to 5-6cm in diameter, usually filled with pus.A lung abscess is a pus-filled cavity located in the lung, surrounded by inflamed tissue. A common reason for the formation of an abscess is aspiration of bacteria originating from the mouth or throat into the lungs, producing an infection.
PARTHENOGENESIS OF Lung Abscess
The formation of an anaerobic lung abscess nearly always Involves two coexisting abnormalities (I) periodontal sepsis such as gingivitis or pyorrhea, which provides the inoculum, and (2) aspiration, which provides access to the lung parenchyma. The usual causes for aspiration are those that compromise consciousness and the gag reflex, such as alcoholism, drug addiction, general anesthesia, seizure disorder. sedative use. or neurologic disorders. Other factors predisposing to aspiration include dysphagia resulting from esophageal disorders or neurologic deficits; disruption of the usual mechanical barriers as with nasogastric intubation, tracheostomy, or nasogastric feeding tubes; or pharyngeal anesthesia as seen with dental procedures or surgery involving the upper airway. Most healthy persons periodically aspirate small inocula from the upper airways, but these are readily cleared by the normal cough reflex and other pulmonary defense mcchanisms without deleterious consequences. Patients who develop aspiration pneumonia and lung abscesses presumably do so because of the relatively large inocula of bacteria and failure of the usual protective mechanisms.
CLINICAL MANIFESTATIONS Of Lung Abscess
Patients with anaerobic abscesses tend to have indolent symptomatology with medical complaints dating for two or more weeks before presentation. The usual symptoms are fever, malaise, cough, sputum production, and pleuritic pain The frequent observation of weight loss and anemia provides testimony to the chronirity of the infection. There may be “chilliness,” but frank rigors arc rare and their presence suggests organisms other than anaerobes. The cough often becomes more productive at the time of cavitation; there may be hemoptysis, and it is at this time that the patient is most likely to note the onset of putrid discharge. Putnd sputum, which is considered diagnostic of anaerobic infection, is found in 60 per cent of patients with a confirmed anaerobic etiology.
Many patients will also note an unusually noxious taste to the sputum. Most patients have a history of compromised consciousness or other risk factors for aspiration, and many have gingival crevice disease Nevertheless, about 10 per cent of patients with anaerobic lung abscess have no identifiable predisposing condition Occasional patients with anaerobic lung abscesses an? edentulous, the incidence of underlying bronchogenic neoplasms seems particularly high in this group.
TREATMENT Of Lung abscess
Obviously. treatment of lung abscess will depend on the underlying cause. For those due to infection, the most important facets of the treatment program are the administration of appropriate antibiotics and adequate drainage of any associated empyema Physiotherapy with postural drainage should be utilized when possible, however, this must be done with considerable caution in patients with large lung abscesses because of the possibility of spillage of purulent contents with extensive involvement of other lobes.
The drugs of choice for the treatment of abscess caused by aerobic pyogenic microorganisms, M. tuberculosis, fungi, and Enttmceht hstoiytic are reviewed in detail elsewhere in this volume. For aspiration-related lung abscess involving anaerobic penicillin has traditionally been regarded as the favored drug on the basis of its long, well-established track record.
There is considerable variation in the dosage recommend at MRS. but most authorities recommend penicillin G in doses of 10 to 20 million units per day This is continued until the patient is afebnlc and dime ally improved, at which time treatment ts changed to intramuscular or oral penicillin using penicillin G, penicillin V, or amptcillin in doses of 500 lo 750 mg four times daily Some authorities suggest a total duration of treatment of three to six weeks, while others base this deciswn on findings with serial radiographs, in the latter instance, treatment is continued until the chest radiograph changes have cleared or there is only a small stable residual lesion This commonly requires two to four months or longer but may be nccrssarv to prevent relapses.
Clindamycin is the ma|or alternative to penicillin This agent is active against most penicillin-resistant anaerobes that are found in 20 to 25 per cent of cases, including many or most strains of B. mclamnogenicm, B. fragtlis. B. rummkom. and B ureolyticum. Some regard clindamycin as the preferred agent for all lung abscesses due to anaerobic bactena. others advocate it only for patients who fail to respond to penicillin, have a contraindication to penicillin, or have a senous infection with a fulminant courso. The usual regimen is 600 mg given intravenously every six to eight hours until the patient is afebrile and clinically improved, followed by 300 mg orally four times daily. Alternative agents with a limited but favorable experience for anaerobic lung abscesses include tetracyclinc and cephalosporins.
These drugs could be used in extenuating circumstances, such as unusual bacteriologic findings or contraindications to both penicillin and clindamycin. The necessity to treat the aerobic component of mixed aerobic-anaerobic infections is controversial, but this is generally advocated for patients who are seriously ill or fail to respond to clindamycin. In selecting regimens for these mixed infections, it is important to note that most penicillins are equally effective against oral anaerobes. This includes penicillin G, penicillin V, ampicillin, amoxicillin, carbenicillin, and piperacillin. However, antistaphylococcal penicillins, such as nafcillin or oxacillin, are considered inferior and unacceptable. Cephalosporins are considered nearly equivalent to penicillins in terms of in vitro activity, although the clinical experience is much more limited than it is with penicillin or clindamycin.
Patients with lung abscesses involving S. aureus should be treated with a penicillinase-resistant penicillin or a cephalosporin. Vancomycin is the preferred agent for methicillin-resistant strains of S. aureus. This agent or clindamycin may be used for patients with a contraindication to beta-lactam antibiotics. Penicillin G is the preferred agent for infections involving group A beta-streptococcal infection. Antibiotic selection for infections involving gram-negative bacilli requires in vitro sensitivity data. This usually consists of an aminoglycoside combined with an expanded spectrum penicillin such as ticarcillin for P. aeruginosa or an aminoglycoside combined with a cephalosporin for En-terobacteriaceae. Sulfonamides are preferred agents for Kocardia infections.
The expected response to antimicrobial agents is subjective improvement with decreased fever within 3 to 7 days and elimination of fever within 7 to 14 days. The putrid odor of the sputum, when initially present, usually resolves in three to ten days. Radiographic response is delayed; in fact there is often extension of the infiltrate and increased cavity size or new cavity formation during the first one or two weeks. However, radiographic evidence of progression after two weeks of treatment usually indicates inadequate response. Chest radiographs should be followed at two- to three-week intervals with the expectation that infiltrates will clear and that there will be a small residual scar or a thin-walled cyst. Compliance to longterm oral regimens of antibiotics among outpatients may be a problem, particularly in the patient population most likely to develop primary lung abscesses.
Bronchoscopy is indicated after a week or two of hospitalization and treatment in patients with an atypical presentation and in those who fail to respond to recommended antimicrobial regimens. The major purpose of the procedure is to detect underlying lesions, such as bronchogenic neoplasms, bronchostenosis, or a foreign body, but it may also be used to facilitate drainage. Other considerations in patients who fail to respond include alternative etiologic agents, the use of alternative antibiotics, and the possibility of an empyema requiring drainage. Nearly all patients respond to antibiotics and do not require surgery.
The major indications for surgery are uncontrollable or life-threatening hemorrhage or a lung abscess that proves absolutely refractory to medical treatment. Medical failures are most common in patients with an obstructed bronchus, those with extremely large abscesses, those with abscesses that have been present for an extended period before the institution of treatment, and those with infections involving certain bacteria such as gram-negative bacilli. The usual surgical procedure is lobectomy. Patients with an inadequate pulmonary-reserve may undergo wedge resection or an external drainage procedure.
PROGNOSIS of Lung Abscess
The natural course of lung abscesses was best studied in the prechemotherapeutic era. Treatment at that time was nearly equally divided between conservative management using postural drainage and supportive care, and surgery. The mortality rate was about 33 per cent in both groups. An additional third of patients developed a chronic debilitating disease or suffered recurrent symptoms. The technique of resectional surgery was developed at about the time penicillin became available and the relative merits of these two approaches as the primary therapeutic modality were widely debated. During the past two decades, however, the majority of patients have been treated with antibiotics alone, including those with “delayed closure” (i.e., the persistence of a cavity demonstrated by a chest radiograph at four to six weeks after the initiation of antibiotic therapy), because most of these cavities eventually resolve if the antibiotics are continued long enough.
The mortality rate for aspiration-related lung abscess is currently reported at 5 to 6 per cent. Findings that herald a relatively poor prognosis include (1) large cavity size, particularly cavities greater than 6 cm in diameter, (2) prolonged symptoms prior to presentation, especially symptoms for over six weeks, (3) necrotizing pneumonia characterized by multiple small abscesses in contiguous segments, (4) patients who are elderly, debilitated, or immunologically compromised, (5) abscesses associated with bronchial obstruction, and (6) abscess due to aerobic bacteria, including S. aureus or gram-negative bacilli.
PREVENTION Of Lung Abscess
The major preventive measures are factors used to reduce the incidence or magnitude of aspiration, appropnate care of periodontal disease, early treatment of pneumonia, and adequate courses of antimicrobials to prevent relapses.
A lung abscess is a localized collection of pus within the lung tissue, usually caused by a bacterial infection. Here’s a guide in tabular format to understand how a lung abscess works:
| Aspect | Description |
|---|---|
| Cause | Usually bacterial infections, often after pneumonia or aspiration of bacteria from the mouth. |
| Risk Factors | Poor dental hygiene, alcoholism, impaired consciousness, immune suppression, chronic lung disease. |
| Pathogenesis | Bacteria enter the lung tissue, causing infection and inflammation, leading to necrosis and pus formation within a localized area. |
| Symptoms | Fever, cough, foul-smelling sputum, chest pain, weight loss, night sweats. |
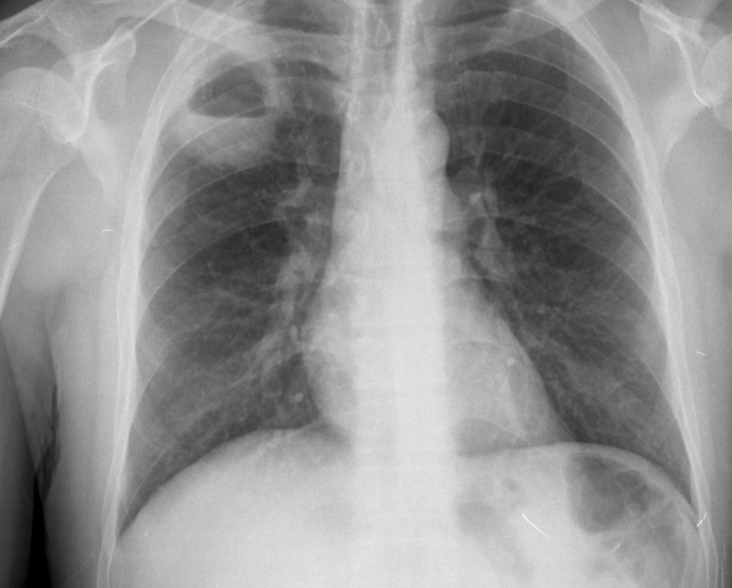
| Diagnosis | Chest X-ray or CT scan to identify the abscess, sputum culture to identify the bacteria. |
| Treatment | Antibiotics to target the specific bacteria, drainage if necessary, supportive care. |
| Complications | Empyema (pus in the pleural space), septicemia (infection in the blood), lung damage. |
| Prevention | Good dental hygiene, avoiding excessive alcohol, vaccination against pneumonia. |
This table provides a general overview, but specific cases may vary. It’s important to consult healthcare professionals for personalized information and treatment.
Conclusion:
By understanding how lung abscess works, you are better equipped to recognize its symptoms, seek timely medical attention, and explore suitable treatment options. Remember, early diagnosis and appropriate treatment are crucial for a successful recovery. If you suspect you may have a lung abscess, consult with a healthcare professional for proper evaluation and care.